Cycling and Running in the Heat #1: The Science
We all struggle in hot temperatures. Cycling and running in the heat is much harder than running in cooler temperatures. In this blog I will consider why; and in part II I will try and quantify the effect in a calculator.
Ideally you should race in moderate conditions if you can, but sometimes this isn’t possible. Races tend to take place in the summer. But you don’t need to fear warm races. Basic guidelines are to slow-down and avoid pushing the pace, drink to thirst, and to dress for the conditions. There are also aero benefits to riding in warmer weather. Today my agenda is:
⚫ To understand the mechanisms of heat exhaustion
⚫ To understand how heat limits performance
⚫ To understand acclimatization to the heatRR
Mechanisms of Heat Exhaustion

When the air temperature is high, the human body uses the evaporation of sweat to cool down, with the cooling effect directly related to how fast our sweat evaporates. To regulate an increasing body temperature, your body sweats and the evaporation process cools the skin through a process called convective heat transfer or convection. Convection is also the reason for feeling much colder when it is windy and why water of 25°C feels much colder than an air temperature of 25°C.
Humans evolved as a hairless ape and one with sweat glands all over our body. This is crucial when running and cycling for long periods. It helps to explain why animals struggle to beat us in the heat. The hotter it is, the better humans are able to run compared with horses. Normal body temp is 97–100F. A 2014 study found a person who is at rest, wearing minimal clothing, in a very dry room and drinking water could probably avoid overheating up to115 degrees Fahrenheit; add a pool of water and a powerful fan, a human could conceivably tolerate heat of up to 140F
Also exercise produces heat, for every 1kcal energy used during exercise 4kcal are produced!
If left untreated exercise can lead to heat stroke, which is characterized by a body temperature of 104°F (40°C) or higher, hot and dry skin, disorientation, and in rare cases, seizures. Heat stroke is a medical emergency and requires immediate medical attention
Rarely sweat production can lead to dehydration if the resultant body water deficits are not adequately replenished. Dehydration decreases blood volume that can eventually exacerbate cardiovascular strain and also lead to acute kidney injury and failure. High internal temperatures (39–40°C), combined with ischaemia and increased oxidative stress after blood redistribution, can cause cell, tissue, or organ damage, with the brain, heart, kidneys, intestines, liver, and lungs at the greatest risk (figure). Heat-derived lung damage, in the form of pulmonary oedema and acute respiratory distress syndrome is also a risk.
However, lesser known than dehydration per se, is that cardiovascular strain is the biggest danger. Changes in cutaneous circulation can significantly augment heat loss — or minimize dry heat gain — during sports and exercise in hot environments. While resting in a thermoneutral environment, about 0.5 L min-1 of blood (5–10% of cardiac output) is supplying the cutaneous circulation, but during heat stress the cutaneous circulation receives up to 8 L min-1(50–70% of cardiac output).
Half of your blood volume is needed for cooling in hot conditions

Heat and Reduced Performance
It is generally accepted that exercise at a constant effort is dangerous once the core body temperature reaches about 40C /111F. However, if subjects are allowed to vary their pace freely, they will preemptively reduce their exercise intensity to prevent their core temperature form reaching the critical point[Tucker 2008,11]. Elevated core temperature reduces the voluntary maximum muscle force generated, though it is unimpaired when electrical stimulation is used, indicating the central nervous system is responsible[Nybo 2008] This is one of the important central governor mechanisms.
When exercising at a constant Rating of Perceived Exertion, subjects steadily reduced their power output between 59f/15c and 77f/25c or 95f/35c even though their perception of their temperature comfort remained constant[Tucker 2006].
Hot conditions reduce V̇O2max and therefore the exercise intensity is effectively increased and in the heat you burn more carbohydrate than in cool conditions[15]. Exercise in the heat also burns more muscle protein [Marino 2001]
Not Just Temperature
Ambient temperature as a stand-alone factor is not an ideal predictor of the integrated environmental heat stress because moisture and wind are important. However, in studies where wind speed, humidity and radiation are controlled (remain constant across trials),33–38 performance and the physiological responses are directly influenced by elevated air temperature, as it will limit dry heat loss and either 1) restrict the upper limit for heat dissipation thereby restricting the exercise intensity that may be endured due to constrained ability to maintain heat balance ) or 2) it will elevate the skin temperature thereby superimposing a cardiovascular restrain on the ability to support the increased need for skin perfusion and maintenance of stroke volume and arterial oxygen delivery to the exercising muscles. The direct and independent effects of humidity,6 wind speed,9,10,40 and radiation on exercise endurance and physiological responses have been verified in laboratory studies with fixed intensity,7,8
Pro cyclists who are well acclimatized (see discussion below) may complete prolonged TT’s in rather hot conditions (36 °C dry air) with maintained performance (i.e., similar or slightly increased average speed) as the lower air density in the heat more than compensates for minor reductions in power output during such conditions.13 In accordance, power output during indoor trials may also be maintained at temperatures up to at least 27 °C when humidity is modest (40% relative humidity) and wind speed corresponds to the movement speed generated during outdoor cycling,38 whereas marked reductions are observed when air movement is minimal. Let’s look at humidity specifically
Moisture effects (Dew Point)
Dew point adversely affects cooling. The rate at which sweat can evaporate depends on how much moisture is in the air and how much moisture the air can hold. If the air is already saturated with moisture, sweat will not evaporate which is why the higher the dew point, the greater the discomfort… higher than normal heart rates and reduced watts. In fact some coaches have combined the two by simply adding them like this
Let’s say the temperature was 84 degrees and the dew point was 60, adding them =144, which according to the calculation below would tell you to adjust your pace by 3%-4.5%.
100 or less: no pace adjustment necessary
101 to 110: 0.0% to 0.5% pace adjustment
111 to 120: 0.5% to 1.0% pace adjustment
121 to 130: 1.0% to 2.0% pace adjustment
131 to 140: 2.0% to 3.0% pace adjustment
141 to 150: 3.0% to 4.5% pace adjustment
151 to 160: 4.5% to 6.0% pace adjustment
161 to 170: 6.0% to 8.0% pace adjustment
171 to 180: 8.0% to 10.0% pace adjustment
Above 180: hard running not recommended
from https://sportcoaching.co.nz/running-in-the-heat-calculator/
OK, next let’s delve into acclimatization.
Acclimatization to High Temps

Some athletes have an unbelievalbe ability to exercise in the hot. Key changes that your body makes with chronic, daily, heat exposure are: an increase in sweat rate and decrease in sweat electrolyte concentration, blood plasma volume expansion, lower skin and core temperatures, lower heart rate during exercise, increased fluid and cardiovascular stability, and a decrease in the metabolic cost of work (exercise)
Blood plasma, which normally makes up 55% of your blood volume, helps to carry not only red blood cells (held in suspension) but also helps to carry and transport nutrients, hormones, and other proteins. The result of an increase in plasma volume (and its carrying capacity) is an increase in cardiac output, or rather, the amount of blood the heart can pump through the circulatory system in one minute (cardiac output = heart rate x stroke volume). The result is a higher VO2max at any given effort level. Studies show that with seven to 10 days of heat acclimation, resting blood plasma volume can expand anywhere from 4.5 to 13% (5,6,7,8).

In an outdoor study by Racinais et al. 14 days of heat acclimatization increased average power output from 256 to 294 W, improving time required to complete a flat 43 km TT from 77 min in the unacclimatized state to 66 min following acclimatization. The ∼40 W increase in average power output post-acclimatization corresponds to an increased metabolic rate of ∼190 W and heat production of ∼150 W, which was counterbalanced by an increased sweat rate of 0.3 L/h. , while the end/peak core temperature and estimated rate of heat storage were unchanged across TT’s in the acclimatized and unacclimatized condition.
Indoor studies by Lorenzo et al.30 and Keiser et al.,34 indicating that trained subjects, both pre- and post-acclimatization, “exhaust” their heat storage capacity during self-paced prolonged exercise in the heat, but utilize the improved capacity for heat dissipation.
However, in a recent meta-analysis, Daanen et al. estimated that improvements in heart rate (HR), core temperature (Tc), and sweat rate decrease by~2.5% per day once individuals are removed from the heat, suggesting that heat tolerance returns to baseline values between 5 and 7 weeks following the process of heat acclimation/acclimatization

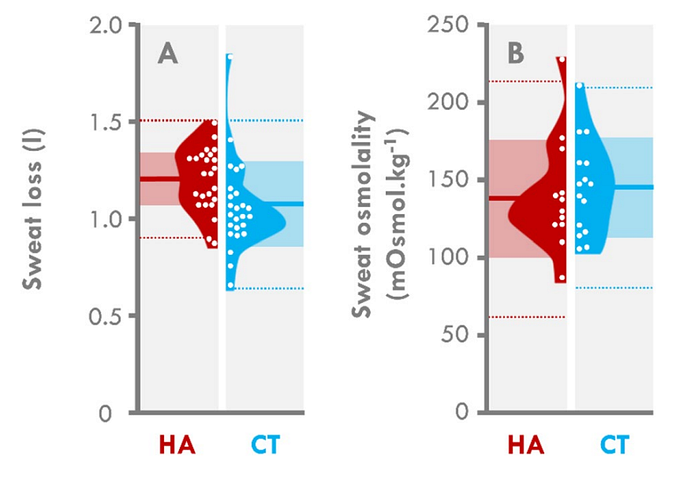
A new study examined the long-term effects of heat acclimatization on the level of heat tolerance. Physiological and subjective markers of heat tolerance were assessed during a heat stress test (HST: 3× 8-min runs outdoors [~ 40 °C and 20% RH] at 50% of their estimated speed at VO2max) performed on the 2nd day upon arrival to the desert military base in the United Arab Emirates after a frst day of mostly passive exposure to heat. Among the 50 male French soldiers, 25 partook in a 4-month military mission in countries characterized by a hot environment ~ 6 months prior to the study (HA). The other 25 participants were never heat acclimatized (CT). Rectal temperature (p = 0.023), heart rate (p = 0.033), and perceived exertion (p = 0.043) were lower in the HA than CT group at the end of HST.
Soldiers who experienced a 4-month heat acclimatization had a higher level of heat tolerance during exercise in the heat, even 6 months later

Guidelines for Exercise in the Heat
- Pace Yourself! If your core temperature gets too high, you can suffer from heat stroke. Runners who get heat stroke typically ignore the warning signs and push on until they collapse. Risk can be high in fast short event where the rise in core temperature can be extremely rapid but generally happen at the marathon distance as well. The key to avoiding heat stroke is to take it easy and don’t push hard (see below on “go slower”), especially if you’re new to running. You should watch out for the warning signs of overheated listed below. Note that some antidepressant medications have been linked to heatstroke.
- Hydrate Carefully. Contrary to expectations, it’s tough to die from dehydration unless you’re running in a remote location. A runner died from dehydration in 2004, but they were running in the Grand Canyon in July where the temperatures can hit 120f in the sun. If you have access to drinks, dehydration is self-limiting. Contrary to popular belief, which has been promoted by the sports drink industry, the evidence is that mild dehydration (<=4%) doesn’t impact performance[1][2]. See The Science Of Hydration for details.

- Don’t over Hydrate! Unlike dehydration, drinking too much is far more likely to be fatal. This condition, called hyponatremia, has killed several athletes over the years. So its usually best to drink to thirst and keep your salt intake high. This will avoid dehydration or overhydration. Adding 1/4 teaspoon of salt to each quart/liter of drink helps may offset electrolyte loss.
- Sunburn. Not only does sunburn cause long-term health issues, it can also cause more immediate problems with your body’s temperature control. Burned skin doesn’t sweat so well in the heat, and in colder conditions burned skin can’t contract the capillaries to reduce heat loss. Cover up, more than you think is needed!
References
Nicklas Junge, Rasmus Jørgensen, Andreas D. Flouris & Lars Nybo (2016) Prolonged self-paced exercise in the heat — environmental factors affecting performance, Temperature, 3:4, 539–548, DOI: 10.1080/23328940.2016.1216257
E. D. B. Goulet, Effect of exercise-induced dehydration on endurance performance: evaluating the impact of exercise protocols on outcomes using a meta-analytic procedure, British Journal of Sports Medicine, volume 47, issue 11, 2012, pages 679–686, ISSN 0306–3674, doi 10.1136/bjsports-2012–090958
E. D. B. Goulet, Effect of exercise-induced dehydration on time-trial exercise performance: a meta-analysis, British Journal of Sports Medicine, volume 45, issue 14, 2011, pages 1149–1156, ISSN 0306–3674, doi 10.1136/bjsm.2010.077966
Roberta S. Erickson, Sharon K. Kirklin, Comparison of ear-based, bladder, oral, and axillary methods for core temperature measurement, Critical Care Medicine, volume 21, issue 10, 1993, pages 1528–1534, ISSN 0090–3493, doi 10.1097/00003246–199310000–00022
?lker Devrim, Ate?? Kara, Mehmet Ceyhan, Hasan Tezer, Ali Kerem Uluda??, Ali B??lent Cengiz, ??nci Yi??itkanl, G??lten Se??meer, Measurement Accuracy of Fever by Tympanic and Axillary Thermometry, Pediatric Emergency Care, volume 23, issue 1, 2007, pages 16–19, ISSN 0749–5161, doi 10.1097/PEC.0b013e31802c61e6
Marianne M. Nimah, Khaled Bshesh, Janice D. Callahan, Brian R. Jacobs, Infrared tympanic thermometry in comparison with other temperature measurement techniques in febrile children, Pediatric Critical Care Medicine, volume 7, issue 1, 2006, pages 48–55, ISSN 1529–7535, doi 10.1097/01.PCC.0000185476.35550.B2
Andrew T. Garrett, Niels G. Goosens, Nancy G. Rehrer, Mark J. Patterson, James D. Cotter, Induction and decay of short-term heat acclimation, European Journal of Applied Physiology, volume 107, issue 6, 2009, pages 659–670, ISSN 1439–6319, doi 10.1007/s00421–009–1182–7
Andrew T. Garrett, Rob Creasy, Nancy J. Rehrer, Mark J. Patterson, James D. Cotter, Effectiveness of short-term heat acclimation for highly trained athletes, European Journal of Applied Physiology, volume 112, issue 5, 2011, pages 1827–1837, ISSN 1439–6319, doi 10.1007/s00421–011–2153–3
R. A. Neal, J. Corbett, H. C. Massey, M. J. Tipton, Effect of short-term heat acclimation with permissive dehydration on thermoregulation and temperate exercise performance, Scandinavian Journal of Medicine & Science in Sports, volume 26, issue 8, 2016, pages 875–884, ISSN 09057188, doi 10.1111/sms.12526
Mark J. Patterson, Jodie M. Stocks, Nigel A. S. Taylor, Sustained and generalized extracellular fluid expansion following heat acclimation, The Journal of Physiology, volume 559, issue 1, 2004, pages 327–334, ISSN 00223751, doi 10.1113/jphysiol.2004.063289
Oliver R. Gibson, Gareth Turner, James A. Tuttle, Lee Taylor, Peter W. Watt, Neil S. Maxwell, Heat acclimation attenuates physiological strain and the HSP72, but not HSP90α, mRNA response to acute normobaric hypoxia, Journal of Applied Physiology, volume 119, issue 8, 2015, pages 889–899, ISSN 8750–7587, doi 10.1152/japplphysiol.00332.2015
R. Tucker, Thermoregulation, fatigue and exercise modality., Med Sport Sci, volume 53, pages 26–38, 2008, doi 10.1159/000151548, PMID 19208997
R. Tucker, L. Rauch, YX. Harley, TD. Noakes, Impaired exercise performance in the heat is associated with an anticipatory reduction in skeletal muscle recruitment., Pflugers Arch, volume 448, issue 4, pages 422–30, Jul 2004, doi 10.1007/s00424–004–1267–4, PMID 15138825
Nybo, Lars. “Hyperthermia and fatigue.” Journal of Applied Physiology 104.3 (2008): 871–878.
R. Tucker, The rate of heat storage mediates an anticipatory reduction in exercise intensity during cycling at a fixed rating of perceived exertion, The Journal of Physiology, volume 574, issue 3, 2006, pages 905–915, ISSN 0022–3751, doi 10.1113/jphysiol.2005.101733
T. Mündel, Exercise heat stress and metabolism., Med Sport Sci, volume 53, pages 121–9, 2008, doi 10.1159/000151554, PMID 19209003
RJ. Snow, MA. Febbraio, MF. Carey, M. Hargreaves, Heat stress increases ammonia accumulation during exercise in humans., Exp Physiol, volume 78, issue 6, pages 847–50, Nov 1993, PMID 8311952
FE. Marino, Z. Mbambo, E. Kortekaas, G. Wilson, MI. Lambert, TD. Noakes, SC. Dennis, Influence of ambient temperature on plasma ammonia and lactate accumulation during prolonged submaximal and self-paced running., Eur J Appl Physiol, volume 86, issue 1, pages 71–8, Nov 2001, PMID 11820326
AR. Hsu, TA. Hagobian, KA. Jacobs, H. Attallah, AL. Friedlander, Effects of heat removal through the hand on metabolism and performance during cycling exercise in the heat., Can J Appl Physiol, volume 30, issue 1, pages 87–104, Feb 2005, PMID 15855685
Amiram Shkolnik, C. Richard Taylor, Virginia Finch, Arieh Borut, Why do Bedouins wear black robes in hot deserts?, Nature, volume 283, issue 5745, 1980, pages 373–375, ISSN 0028–0836, doi 10.1038/283373a0